Urethral catheters
Catheters can be indwelling or intermittent self catheters.
Indications:
Urinary retention - acute or chronic
Monitoring urine output
Peri-operative period
Patients indefinitely requiring a long term catheter mainly in neurological conditions such as MS/stroke/demyelinating conditions
Patient and carer preference to manage incontinence
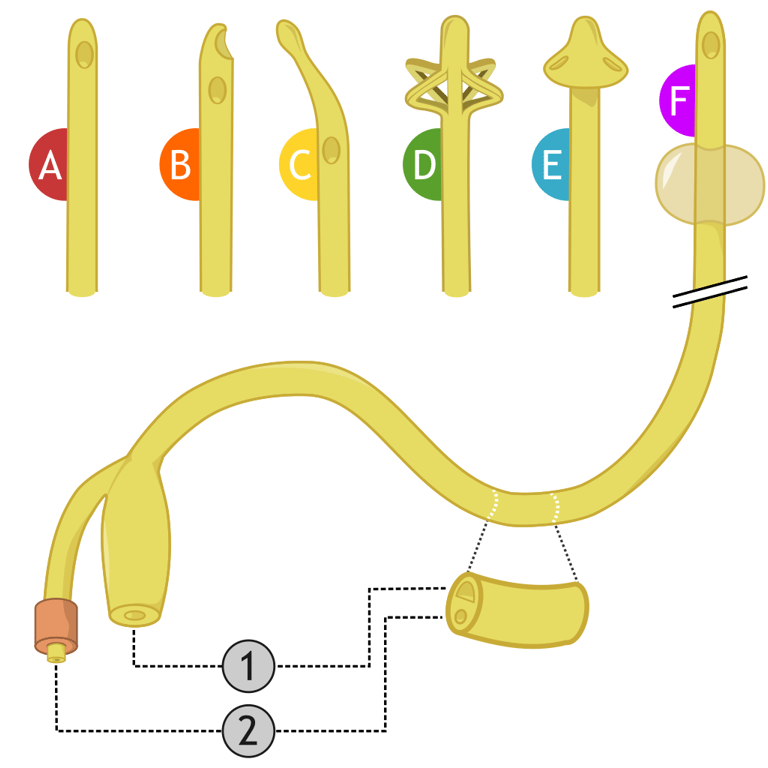
The following are the most commonly encountered types of indwelling catheters:
Latex catheters - Brownish yellow short term catheters (up to 28 days.)
Silicone catheters - transparent - the standard long term catheter (up to 12 weeks.)
Tiemann tip catheters - a slightly curved tip allows bypassing a bulky prostate. This catheter should always be introduced with the tip pointing at 12 o clock and this position maintained throughout the procedure. There is a limited role for this type of catheter in females.
Standard 3 way catheter - used in haematuria for continuous bladder irrigation and bladder washouts.
Coude 3 way catheter - similar to the Tiemann tip catheter, the coude 3 way has a soft curved tip allowing the operator to bypass the prostate. Used in haematuria for continuous bladder irrigation and bladder washouts.
Council tip catheter - an open ended catheter for specialist use. Allows the catheter to be inserted over a guidewire - useful in difficult catheter scenarios.
Image 1 - types of catheters. A - Standard catheter, B - Open ended / whistle tip catheter, C - Coude / Tiemann tip catheter, D - Nelaton catheter, E -Muschroom catheter, 1- Drainage port, 2- Balloon port
Risks associated with urethral catheter insertion / indwelling catheters:
Catheter associated UTI
Urethral trauma / strictures
Erosion hypospadiasis
Discomfort
Paraphimosis
As the number associated with a catheter size described in French (Fr) increases, so does the internal diameter (in contrast to intravenous cannulas)
Choosing the right size:
Non haematuria setting:
A 14Fr catheter in men
A 12Fr catheter in women
In the haematuria setting:
A 20 Fr catheter at the very least is advised. The wider internal diameter allows washouts and clot evacuation / drainage
Top tip - some hospitals may use male (longer) and female (shorter) catheters. Check the product information. If in doubt, you're better off using a male (longer) catheter in all cases.
Using a female catheter in a male will risk urethral trauma and cause bleeding once the balloon is inflated as it would sit distal to the bladder neck.
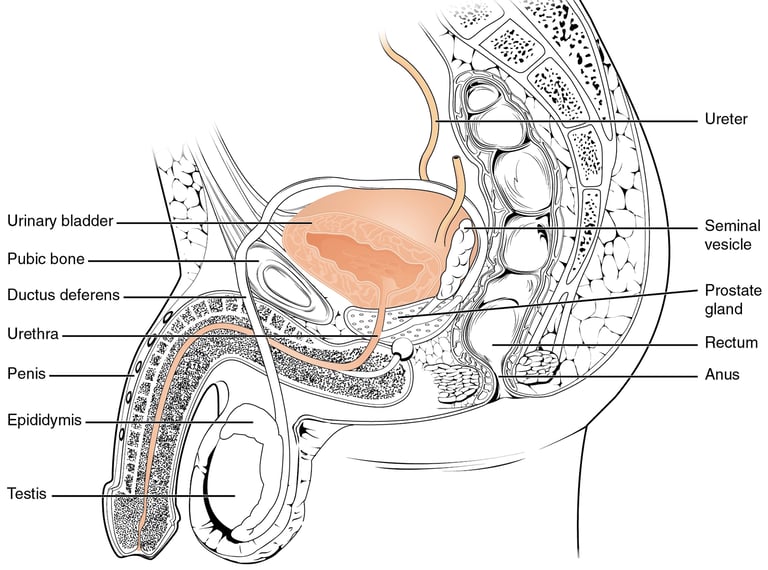
Catheterisation and anatomy
The male urethra is ‘S’ shaped and is roughly 18 - 22 cm in length
The female urethra is straight and is much shorter at about 3 - 4 cm in length
The ‘S’ shaped nature of the male urethra is the major difference and not appreciating this will lead to multiple attempts of failed catheterisation, discomfort and trauma (to both the patient and operator)
Figure 1 - anatomy of the male urethra
Male catheterisation:
Consent
Position the patient supine
Don sterile gloves
Prep the penis using chlorhexidine prep - soak the cotton balls in the solution and using the forceps provided in a catheter pack thoroughly clean the glans, retracting the prepuce and cleaning the coronal sulcus. Be generous with the use of solution and cotton balls as it will prevent or minimise infections
Place the drape over the site with the cutout for the penis, give the drape a shake to get the penis over it onto a sterile field
With the left or nondominant hand, grasp the penis between the middle and ring finger and stretch it upwards towards the ceiling (perpendicular to the bed)
Use the prefilled lubricant syringe to instill lubricant which ideally would contain an anaesthetic such as lignocaine. Squeeze out a drop or two of jelly onto the urethral meatus before inserting the tip of the syringe for extra comfort. Warn the patient that it will sting for couple of minutes
Push down on the plunger slowly and empty the syringe
After 2 minutes, insert the catheter. Gently introduce it down the urethra with the penis stretched as far as possible towards the ceiling; guiding the catheter on its way down with your left thumb and index finger
The first anatomical narrowing is the membranous urethra. Ask the patient to take deep breaths and you
At the point of resistance, apply gentle pressure as you advance the catheter and drop the penis down to bring it almost parallel to the bed. This should help introduce it further
Advance the catheter upto the hilt (the junction of the 2 or 3 ports)
Ensure that urine is draining out of the catheter. This is a good time to get a catheter sample of urine if needed. If nothing comes out - gently aspirate with a bladder syringe or the syringe used to insert the lubricating jelly. This step clears out the jelly blocking the catheter
Inflate the balloon only if urine comes out. A standard catheter will require 10ml of distilled water to inflate the balloon whereas 3 way catheters usually indicate the volume on the drainage port and 20-30ml is a standard volume.
Connect the urine bag
Always replace the foreskin to avoid a paraphimosis
Video 1 - male urethral catheterisation.
Female catheterisation:
Catheterising females is much more straightforward. Prep the labia and vagina well. With good lighting locate the urethra and instil about 5ml of lubricant/anaesthetic jelly. Insert the catheter gently until urine begins to drain. The length of insertion is about 8 cm or less.
Positioning a female patient is important - ask the patient to bend their knees and bring their ankles towards the buttock as close as possible before dropping the knees off onto either side. Reminding the patient that the position is similar to a “smear position” could be a useful aid.
Common issues faced during catheterisation and workarounds
Cannot get beyond the prostate - At the point of resistance drop the penis down to bring it almost parallel to the bed. This should help introduce it further.
Still cannot get beyond the prostate - Use a Tiemann tip catheter
Bleeding after catheterisation - this is likely urethral and will settle over the next hour or two. Counsel the patient and reassure them that it will subside.
No urine coming out once inserted - If there isn't any urine coming through, using the empty lubricant syringe, place it into the outflow port with a good seal and pull on the plunger. This usually works to displace the jelly blocking the catheter and urine should follow thereafter.
Blocked catheter - before removing a catheter just because it’s blocked, try flushing it first. Debris may very well block the catheter and a good washout will solve the problem and minimise chances of infection by reinserting a catheter. You can also try deflating the balloon, pushing the catheter in, flushing it and reinflating it.
Catheter bypassing - Can be caused by a blocked catheter or bladder spasms. Check the volume of water in the balloon. Make sure that it is the recommended volume. Deflate the balloon, push the catheter in further, flush the catheter and inflate it.
Catheter bypassing with lower abdominal pain (bladder spasms) - Try Solifenacin or Mirabegron. Please read up on the side effects of both these drugs on BNF such as dry mouth and the risks of orthostatic hypotension and falls and counsel the patient. Contraindications include glaucoma and myasthenia gravis.
Phimosis - a non retractile foreskin can make visualisation of the urethra impossible. Insert 1-2 tubes of instillagel to “balloon” the foreskin. Remember that the urethral meatus lies ventrally (at the bottom) of the penis. Use a normal silicone catheter in these cases as they are slightly stiffer. Insertion into the urethral meatus in this case is bline and is done by gently probing with the catheter using your fingers externally to guide it inferiorly. You will immediately know that you are in the urethra when you feel a give and the catheter passes in with ease. Artery clips can be used to stretch out the foreskin and buy some space. This is generally tolerated very well and does not need an anaesthetic however ensure that the rip of the instrument is just below the skin and not accidentally within the urethra.
Elderly females - Difficulty arises primary due to poor positioning or because of atrophic changes of the urethral meatus and vagina. Good lighting and an assistant will generally suffice. Techniques such as finger occlusion of the vagina to guide the catheter above it into the urethral meatus may be needed and verbal consent must be obtained.
Unable to catheterise:
Phimosis - If the above steps fail, If this is not achievable, a flexible cystoscope may be needed to locate the meatus and pass a wire. If unable to do so, a dorsal slit may be required.
A catheter introducer may be used if experienced in the technique. This is a slender, metallic disposable bougie inserted into the catheter ex-vivo to help stiffen it and bypass the prostate.
If the resistance is distal (closer to the meatus) - think of strictures / false passages. In these cases, a flexible cystoscope, a hydrophilic tipped guidewire, urethral dilators and an open ended catheter insertion will become necessary. This must not be performed if you lack the experience to proceed.
Last resort - Suprapubic catheterisation ideally under ultrasound guidance to avoid the risk of inadvertent bowel injury.
Sometimes less is more. Avoid overambitious trials of catheterisation which only risks trauma and causes pain and apprehension - all of which make the procedure harder for a registrar or consultant.
Common catheter related problems (and how to solve them)
Blocked catheter
Expelled catheter
Blood in catheter
Difficulty re catheterising
Pain and bypassing
Formation of bladder stones secondary to the SPC which acts as a foreign body
Management of common problems:
Blocked catheter - Flush gently with 10-20ml. This will usually dislodge the debris and allow the catheter to drain. If the catheter has been in for a while and is due a change then replacement of the catheter with an aseptic technique will resolve the problem.
Expelled catheter - Usually noted when a patient with a weak abdominal wall has a bout of coughing or severe bladder spasms, displacing the balloon and catheter. Needs to be replaced ASAP.
Blood in catheter - Assess for symptoms of a UTI. A urine dip from the catheter is a poor measure of infection as it will almost always be leukocyte and nitrite heavy with white cells detected. If the patient does not have features of an infection, it is worth referring the patient to a haematuria clinic for full assessment. Bladder stones can also cause haematuria and a bladder or upper tract cancer must be considered (see our section on visible haematuria for more details.)
Difficulty re-catheterising may be due to poor technique/ lack of confidence in performing a catheter exchange or because the tract has stenosed or has been lost. In this case a guidewire may be a useful adjunct (if used correctly) to find the tract and railroading a catheter over. If you have any difficulty, it is best to speak to the urology registrar for advise.
Pain and bypassing is often due to bladder spasms - a simple anticholinergic will relieve this and mirabegron may be used at the lowest possible dose.
Bypassing from the urethra can occur and as long as good volumes of urine are passing via the SPC, the patient can be reassured and is likely due to low resistance at the urethra. If high volumes of urine are passed per urethra, consider a blocked SPC and managed as described above.
Persistent bypassing can be assessed in the outpatient setting with appropriate cystometry.Bladder stones - a catheter forms a nidus for stone formation. A stone can cause haematuria and spontaneous expulsions of the catheter due to ruptures of the balloon from caused by the stone.
Unable to deflate the balloon [1-2]:
Balloon port failure - in long term catheters, the balloon port valve may fail. Sometimes, the little release button within the port does not get pushed down by a syringe alone. First, try inflating the balloon with an additional 5ml of water followed by aspirating the contents of the balloon. Avoid overinflating to burst the balloon as fragments of the balloon may remain within the bladder forming a nidus for stones and infection.
If unsuccessful, the back (hard end) of a standard wound or COVID swab can be used to push down on the button which releases the water held within the balloon
If this fails, the balloon port can be cut just below the valve to release water
If step 3 is unsuccessful, the stiffer back end of a wire can be passed along the port to dislodge any crystal deposits along the path of the channel
If this is unsuccessful, a 22G spinal anaesthetic needle can be passed over the guidewire and into the balloon itself to drain the water.
If all of the above fails, needle puncture of the balloon may be needed under ultrasound guidance by the urologist or interventional radiologist. A transabdominal or transrectal approach can both be used.
In women, traction on the catheter balloon may bring it into view through the urethral meatus. A needle can then be used to puncture the balloon.
References:
[1] - https://www.aafp.org/pubs/afp/issues/2000/0915/p1397.html#:~:text=The%20primary%20reason%20for%20the,kinking%20of%20the%20inflation%20channel.
[2] - Giovannopoulou, E., & Chondros, K. (2017). A technique for non-deflating balloon catheter removal in female patients. The Pan African medical journal, 26, 222. https://doi.org/10.11604/pamj.2017.26.222.12291
Images and videos:
Image 1 - Used under the Creative Commons license - OpenStax Anatomy and PhysiologyOpenStax, CC BY 4.0 <https://creativecommons.org/licenses/by/4.0>, via Wikimedia Commons
Video 1 courtesy - Geeky medics - https://www.youtube.com/watch?v=hKiakPX6AdQ
UroMate
contact@uromate.com
© 2025. All rights reserved.
Disclaimer: The content on UroMate is intended for educational use by medical professionals only. It does not constitute professional medical advice, clinical guidelines, or a substitute for supervision or training. UroMate is not an official authority and accepts no responsibility for clinical outcomes. This site reflects UK clinical practice and may not apply elsewhere. Users must consult official sources such as NICE, EAU, or NHS protocols. Medical knowledge evolves, and while we strive for accuracy, content may not reflect the latest guidance. Not intended for patients or the general public. By continuing to use this site, you acknowledge and accept these terms.