Priapism
Priapism is defined as an unwanted erection lasting more than 4 hours in the absence of sexual stimulation that persists despite orgasm or ejaculation.
Types:
Ischaemic (low flow / venous)
Non-ischaemic (high flow/arterial)
Stuttering
Low flow/ischaemic priapism
Veno-occlusive, whereby blood in the corpora cavernosa does not drain. Painful rigidity with a soft glans.
High flow/non-ischaemic type
High inflow of arterial blood with a slow venous drainage. Painless semi erection with a firm glans. Patients may sometimes provide a history of sexual stimulation.
Stuttering priapism
It is a subtype of ischaemic priapism and may very well lead to an ischaemic episode. There is a period of painful erection with spontaneous detumescence.
It is not unusual for the cause of priapism to not be identified. While common causes are listed below, consider possibilities such as pelvic malignancies.
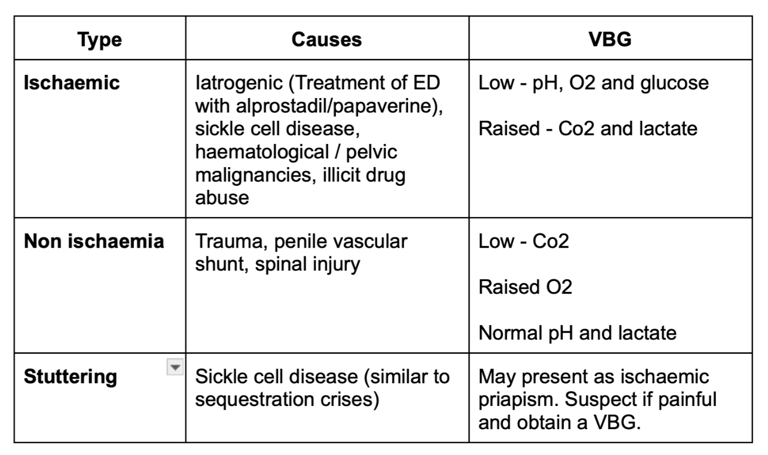
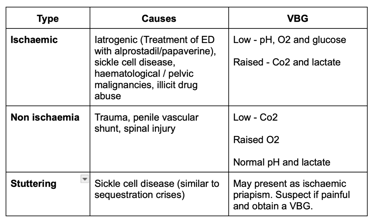
Image 1 - comparison of the types of priapism, causes and VBG findings.
Investigations:
Routine bloods - FBC, U&E, Clotting screen
Drug screen
Blood film (to rule out sickle cell disease)
Colour Doppler to assess perfusion
Abdominal imaging - CT/MRI (especially in idiopathic priapism)
Chest X-ray - in idiopathic priapism
Penile imaging - MRI to assess perfusion, which will also help in planning for a penile prosthesis
As an SHO on urology, inform your registrar as soon as possible once a patient with a possible ischaemic priapism has been referred.
In case of delays and if confident in doing so, steps 1-3 below can be attempted. You may also help prepare the phenylephrine to save time while your senior is on their way.
Management:
Conservative time buying measure - ice packs (ask a colleague to arrange this while you gather the equipment to manage the case)
Dorsal penile block - this is not therapeutic and is only to provide anaesthesia for aspiration. 10ml of 1% lignocaine WITHOUT adrenaline
Cavernous aspiration and washout with a large-bore butterfly needle - aim perpendicular to the midshaft to avoid the corpus spongiosum and urethra. Aspirate 10-15 mL (to be sent for blood gas analysis). Repeat the aspiration and washout with 10ml of normal saline after each aspiration. Continue till the bright (oxygenated) blood can be aspirated. Roughly 30% of priapisms will subside after aspiration.
Failed aspiration - Intracavernosal instillation of a phenylephrine
Failed instillation of phenylephrine - will require surgical shunting
Preparing phenylephrine:
Either dilute the 1-mL phenylephrine ampoule (10 mg) in 49 mL of normal saline using
a 50-mL syringe and use 1-mL aliquots (200 μg) at a time. Alternatively, dilute the 1-mL ampoule in 19 mL normal saline, which is the equivalent of 500 μg/mL. With this dilution, use 0.5 mL of the solution as an aliquot (250 μg).Ensure that the patient has blood pressure monitoring whilst administering phenylephrine.
Use 1 mL of the solution (200 or 250 μg) for injection directly into the corpus cavernosum at the 3 or 9 o’clock position, therefore avoiding the urethra and dorsal neurovascular bundle.
Repeat after 10 min up to a total dose of 1000 μg, provided that there is no significant systemic hypertension.
Complications:
Fibrosis
Erectile dysfunction
References:
https://pubmed.ncbi.nlm.nih.gov/29960632/
https://www.baus.org.uk/_userfiles/pages/files/professionals/sections/andrology/Priapism.pdf
https://teachmesurgery.com/urology/other/priapism/
Images:
Image 1 - Copyright Uromate
UroMate
contact@uromate.com
© 2025. All rights reserved.
Disclaimer: The content on UroMate is intended for educational use by medical professionals only. It does not constitute professional medical advice, clinical guidelines, or a substitute for supervision or training. UroMate is not an official authority and accepts no responsibility for clinical outcomes. This site reflects UK clinical practice and may not apply elsewhere. Users must consult official sources such as NICE, EAU, or NHS protocols. Medical knowledge evolves, and while we strive for accuracy, content may not reflect the latest guidance. Not intended for patients or the general public. By continuing to use this site, you acknowledge and accept these terms.