Haematuria
Haematuria can be of two types
Visible haematuria - visible to the naked eyes with or clots
Non visible haematuria which may be either symptomatic or asymptomatic
Visible haematuria will usually (but not always) require in hospital review for the most part whereas non visible haematuria is often referred to urology outpatients for assessment and management.
Painless visible haematuria is to be considered as bladder cancer until proven otherwise.
Patients may attend with one of the following:
Blood stained urine, small / no clots and able to void urine
Blood stained urine with clots and able to void urine
A recent history (hours to days) of haematuria with clots now in clot retention
Haematuria and feeling poorly
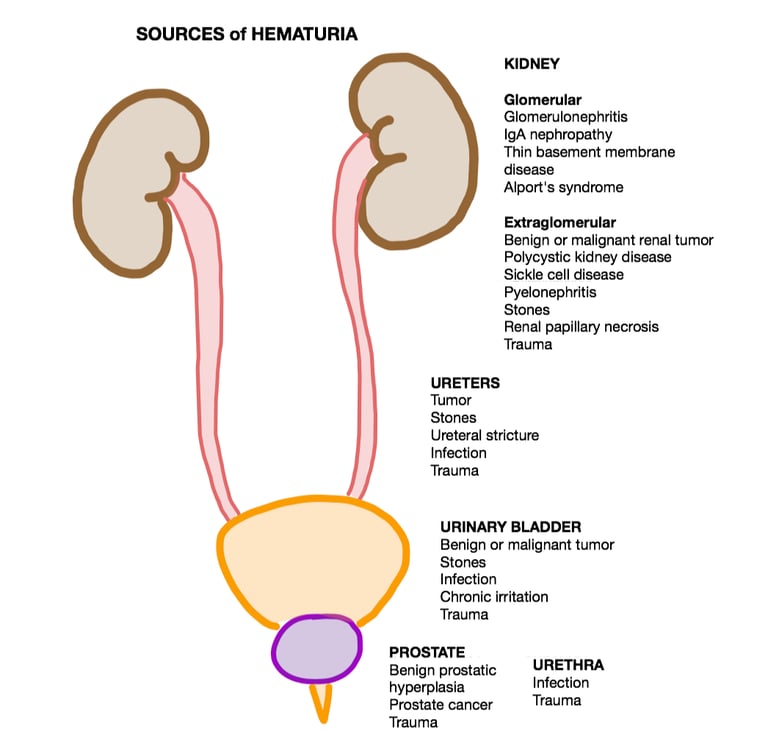
Causes:
Infection - UTI, prostatitis, pyelonephritis
Prostate - BPH / Prostate cancer (Prostates are highly vascular and have a tendency to bleed)
Renal / ureteric / bladder calculi - usually non visible haematuria
Bladder - cancer, radiation cystitis, schistosomiasis
Renal cancer
Iatrogenic
Trauma to the urinary tract
Medication - Warfarin, NOACs and antiplatelets, cyclophosphamide
Nephrogenic causes
Figure 1 - Sources of haematuria
Consider the presentations to determine the safest management plan:
Blood stained urine, small / no clots and able to void urine - Can be discharged home with outpatient workup and safety netting advise.
Blood stained urine with clots and able to void urine - Can be discharged home unless multiple or large clots in which case a bladder washout would be needed to prevent representation with painful clot retention.
A recent history (hours to days) of haematuria with clots now in clot retention - Will need a 3 way catheter, a thorough bladder washout and irrigation until the urine is clear.
Haematuria and feeling poorly - will need admission and management of the cause - antibiotics / irrigation / cystoscopy and clot evacuation.
Investigations:
-Routine bloods including an INR and group and save
-Urine for culture and sensitivity
-Imaging - Ultrasound KUB / CT Urinary tract with contrast
-Endoscopy - flexible cystoscopy
Management:
As with any bleeding scenario, ensure that the patient is safe, assess from A-E and ensure that a valid group and save have been obtained.
Choose the right 3-way catheter (Minimum 20Fr in men, 18Fr in women, Coude tip 3-way for enlarged prostates.)
Perform a thorough bladder washout - use at least 1 Litre of water and evacuate all clots. There is no hard and fast rule as to how much fluid should be used for a washout. A good washout will use as much fluid to gently agitate, break and clear out the clots until the urine is pink/clear / clot-free by the end of the washout.
After washouts have been performed, start on continuous bladder irrigation.
Stop irrigation the following day and review the colour of urine before a TWOC.
Persisting haematuria not responding to ward-based management will benefit from an early cystoscopy + cystodiathermy.
Video 1 - Demonstration of bladder washouts.
The cause of haematuria needs to be assessed and managed accordingly:
A CT scan of the urinary tract with contrast and a flexible cystoscopy is the bare minimum in cases with no obvious cause. The suspicion of a kidney / ureteric / bladder cancer must be at the top of the list of differentials.
In the case of infections, a urine sample for M/C/S and empirical antibiotics can be started based on trust protocol until sensitivities return.
Medication - If sensible to do so, withholding the culprit medication for 24 hours and encouraging increased fluid intake will often resolve the episode of haematuria.
Iatrogenic - usually follows traumatic catheterisation and resolves within a few hours. A hallmark of urethral trauma from an ambitious attempt to catheterise is fresh blood bypassing the catheter, which will usually resolve spontaneously.
BPE / Prostate cancer - Tamsulosin and Finasteride can be started. Finasteride has the added benefit of lowering the vascularity of the prostate in the intermediate to long run. Repeated episodes of BPE-related haematuria will need intervention (TURP or embolisation.)
Urinary tract injury - A registrar or consultant review is mandatory.
Renal cancers - an ultrasound KUB may show a sinister lesion in the kidney, which should be followed by a CT urogram to assess the lesion further, which is the gold standard.
Bladder cancers - Flexible cystoscopy +/- rigid cystoscopy and biopsy / Transurethral Resection of Bladder Tumour.
If cystoscopy and imaging do not yield a cause for haematuria, request a urine ACR and refer to nephrology for further workup.
Images and videos:
Image 1 - Used under the Creative Commons license - Copene, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons
Video 1 - Courtesy of Craig Hospital - https://www.youtube.com/watch?v=13eHF0BqBmY
UroMate
contact@uromate.com
© 2025. All rights reserved.
Disclaimer: The content on UroMate is intended for educational use by medical professionals only. It does not constitute professional medical advice, clinical guidelines, or a substitute for supervision or training. UroMate is not an official authority and accepts no responsibility for clinical outcomes. This site reflects UK clinical practice and may not apply elsewhere. Users must consult official sources such as NICE, EAU, or NHS protocols. Medical knowledge evolves, and while we strive for accuracy, content may not reflect the latest guidance. Not intended for patients or the general public. By continuing to use this site, you acknowledge and accept these terms.